Some of the most important unknowns with COVID-19 are as follows:
- Do we know for sure if a person is immune to COVID-19 after infection?
- What percentage of the U.S. population will be immune after this first wave of infections is over?
- Will immunity last over time, or will it fade?
- If and when a vaccine can produce immunity and stop the pandemic?
It’s helpful in thinking through these questions to understand how the immune system and immunity testing work. A viral infection begins when a virus enters a cell of your body. For the SARS-CoV-2 virus, which causes COVID-19, the spike protein on the viral surface attaches to a cell via a protein receptor on the cell’s surface called ACE-2 and lets itself in. The virus hijacks the cell’s machinery to make copies of itself. Those copies break out of the cell and then spread around your body. The viral copies enter more cells and make more copies, resulting in the death of the cells and disease.
The first type of immunity is known as the innate immune response. This is the base-level protection that everyone has to defend against infections even those the body has never seen the virus before. Once the virus is found, your cells “start secreting cytokines (signaling molecules)” to tell the neighboring cells that there’s a viral infection. Cytokines promote inflammation throughout the body. Inflammation is something that can make you feel sick, but it can also help stop the disease by killing the virus and/or attract cells and molecules that aid in the healing process.
Viruses have evolved ways to counter this initial response. Sometimes viruses produce so many cytokines that they trigger white blood cells to turn against healthy cells that can then lead to organ failure and death in a term called “cytokine storm.” It is unclear why some people develop this storm and not others, though there are indications that aging is a factor, as are underlying conditions like high blood pressure, diabetes or other conditions, which may alter immunity. With COVID-19 this “storm” can occur in the lungs, kidneys, brain, eyes, mouth, nose and even the skin on the toes.
The second type of immunity is called acquired immunity. With this type of immunity, the body actively secretes protein called antibodies. Antibodies are protein molecules that can kill viruses or, in the case of COVID-19, they block the attachment of the virus to the cell receptor. Antibodies are highly specific and can only interact with the virus, which induced the reaction. Antibodies against the SARS-CoV-2 virus are mostly found in the plasma (serum) and it can take from five to 10 days to be detected by most laboratory (serological) tests. However, research has shown with most viral infections can take up to two weeks to clear the virus.
However, not all antibodies can neutralize viral infections. In fact, some antibodies provide no useful propose. Therefore, detecting antibodies, which can react with SARS-CoV-2 virus may not tell the whole picture. Scientists need to perform additional tests to determine if those antibodies are functional against the virus.
Antibody tests
There are two main types of antibody tests. The first looks for antibodies and can be completed quickly. This is called an ELISA test (short for Enzyme Linked Immunosorbent Assay). This test doesn’t provide the most complete picture of immunity. Currently there are 250 kits available that use an ELISA, with sampling that can be done in testing areas or in cases in home using a small drop of blood; however, the FDA has only verified the validity of 12.
The second test is called a serum neutralization test, and it takes a few days to process and requires a larger amount of blood. It not only looks for antibodies, but also measures the ability of the antibodies to prevent the infection of a known amount of virus in destroying living cells in culture. Ideally, scientists will correlate the two tests and figure out which concentrations of antibodies that confer the highest level of immunity. It’s still not known what levels of antibodies are needed to have lasting, protective immunity. What also remains to be shown is whether the presence of antibodies means you can’t give the virus to someone else.
These tests are useful, but they don’t answer everything. As noted earlier, it takes days, if not weeks, for the body to produce antibodies, therefore a negative antibody test doesn’t mean the virus isn’t present. Since antibodies are produced during an infection and linger after it’s cleared, a positive antibody test doesn’t mean that the virus is no longer active.
However, deploying these tests will help answer a lot of questions. Most basically, it can help a person know if they have been exposed to SARS-CoV-2 virus. On a larger scale—if deployed in well-designed studies—serological tests could reveal the complete picture of the pandemic. They can also help scientists answer basic questions like:
- How many people infected with the disease die?
- What percentage of the population has been infected?
- Who, and how many, may have spread it without knowing?
Serological tests could also potentially allow people who have immunity to return to work. That could be a huge boost to front-line health workers who may have been exposed to the virus, but are desperately needed back in action. Even if people do become immune, one thing that is not known is how long that immunity would last. That’s unfortunately not something that can determined until years of testing.
Scientists don’t understand why for some viral infections, your immunity never wanes. People who are immune to smallpox, for example, are immune for life. Less reassuring is that scientists have observed antibody levels to other coronaviruses (there are four coronavirus strains that infect people as the common cold) can last over a period of years. With the SARS virus infection antibodies can be detected in humans after four years and with MERS one year. These two are related coronaviruses, which have caused recent pandemics. However, no one can say at this time what the duration of immunity will be against the SARS-CoV-2 virus.
Over the long term, the immune system becomes less effective with advancing age and these older individuals can acquire more chronic illnesses that can hamper the response to a virus, even if their immune system recognizes. It will be years before scientists can understand what aging means for immunity to COVID-19.
Another problem seen with coronaviruses, is that their genome is unstable and mutations in the spike protein can occur. These mutations may lead to vaccination failure since the antibodies produced by a vaccine may not recognize the mutated spike protein. As is the case with influenza viruses new vaccines may need to be developed at regular intervals, which may take years to be determined. As of yet no such mutations in the SARS-COV-2 virus have been identified.
The CDC, various states and universities, medical research centers and governmental facilities around the world are now conducting serological surveys for SARS-CoV-2 viral antibodies. The tests are being done in public places in volunteers, which have never shown COVID-19 symptoms in an attempt to figure out who was previously infected with the virus. A survey like this can show the actual background rate of infection and answer critical questions like what proportion of people have been infected without showing symptoms and where the virus has spread in a population and quantify the overall rates of severe complications. Knowing these variables can help health officials better target interventions. This “contact tracing” is where trained staff interview people who have been diagnosed with COVID19 or tested positive with an antibody test to figure out who they have recently been in contact with. Then, they communicate with those people that may have been exposed to the virus, encouraging them to quarantine and/or be tested for the virus to prevent spreading the disease any further. It is part public health work and part investigation.
Preliminary results using antibody testing indicate that as many at 10 times the number of people have been infected, then the number of people that have been diagnosed with the disease. A medical term R0 tells the number of persons, which one person can infect. Current estimates of this value are between one and two depending on the geographical location of the outbreak. For a pandemic to be halted requires an R0 less than one.
Convalescent plasma
Another tactic under investigation is using convalescent plasma. The idea is to harvest the liquid part of blood, including proteins used for clotting, from people who have survived COVID-19. This plasma contains antibodies to the virus, so scientists are seeing whether it can help people with active infections get better. Researchers are also studying whether convalescent plasma can be used as a prophylactic to prevent COVID-19. Preliminary results so far are encouraging.
Researchers are also developing monoclonal antibodies in the laboratory against the virus in mice using genetically engineered systems. These antibodies could also be used to treat or prevent the disease. But antibody transfusions, whether they come from COVID-19 survivors or were created in a lab, only confer protection against the virus for a few months.
Long-term strategy of herd immunity
The long-term strategy is to have enough people in a population immune to the virus so that it no longer spreads easily. This is known as herd immunity. It usually requires between 70 and 90 percent of a group of people to be effective, depending on the contagiousness of the virus. Current estimates are that at least 70 percent of the population needs to have been infected to stop the COVID19 pandemic. With a large enough share of immunity in the population, even the remaining people who are not immune face a much lower likelihood of being infected. With few susceptible people in close proximity, pockets of infection quickly fade out.
Herd immunity can be achieved through vaccination or natural infection. According to the World Health Organization, there are currently 102 vaccines which are being developed by laboratories around the world using a variety of techniques, which have been used in the past to develop vaccines against both the SARS and MERS viruses. President Trump recently said he was personally in charge of “Operation Warp Speed” to get 300 million doses into American arms by January, which is a bold challenge indeed. Already, the administration has identified 14 vaccine projects. Combing resources of fewer research groups using different molecular platforms makes good sense.
An ideal vaccine would be molecular based containing only a portion of the spike protein gene and produce immunity in at least 90 percent of the recipients after only one application with only minimal adverse reactions in a small percentage of recipients. It will also need to prevent replication of the virus (sterile immunity) and provide this level protection for at least one year. However, it will need to be determined if a booster administration is needed especially during the first year of use.
There are eight vaccines currently being tested in humans in five different countries. This is necessary if countries limit their early vaccines to their own population. Commercial vaccines are normally licensed in three phases. The first two are primarily for safety and the three for protection (as measured by the ability to produce neutralizing antibodies). This process normally takes from 12 to 18 months to complete. Two of the aforementioned vaccines are now entering phase two. Due to the necessity to rush this vaccine into the market to prevent the world’s economy from collapsing, this entire process has been accelerated and scientists hope to have a safe efficacious vaccine for first responders by the end of the year and for the general population sometime next year. However, the timing for the production and distribution of a vaccine for this goal to achieve herd immunity is unknown since the medical infrastructure for viral or antibody testing and administration of a vaccine in underdeveloped countries is poor and hampered by poverty, governmental corruption, war and lawlessness. In addition, even in developed countries, a mistrust for scientific and vaccination data is often communicated through social media. Estimates to vaccinate 70 percent of the world population may exceed $25 billion.
One thing that is accepted by most scientists and medical experts is that rushing too fast to approve and distribute a vaccine is a gamble since the vaccine(s) may not provide effective long-term immunity and may cause as yet unknown adverse reactions. In addition, some companies are willing to perform a challenge infection, which intentionally infects young, vaccinated volunteers with live SARS-CoV-2. However, this is dangerous, because no one can say what the virus will do in people if the vaccine does not work. These challenge studies have been successfully undertaken in several monkey species in the lab, but how this translates in humans is unknown.
There are presently a number of companies in several countries that are building facilities to mass-produce a commercially licensed vaccine. However, there is probably no need to vaccinate the entire population, because in a year at least 20 percent of the world’s population could have already been to be exposed to the virus. The caveat of not finding a successful vaccine by next spring is that it will take some time in 2021 or 2022 before we reach heard immunity. If that is the case, then plan B to develop and test antivirals in sick humans becomes a necessity to treat the 100s of millions of people who will become seriously ill due to COVID19.
Obliviously there are many questions that have been answered about this virus over the past four months, however, there are many more that have remain unanswered. How fast we answer these remaining questions no one can say.
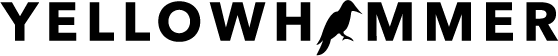
Joseph Giambrone is a professor emeritus in Auburn University’s Department of Poultry Science with a joint appointment in the Department of Pathobiology in the College of Veterinary Medicine. During his graduate research career at the University of Delaware, he was part of a research group that developed the first vaccine against an antigenic variant of an avian coronavirus. During a sabbatical leave during his tenure at Auburn, he was part of a research group in Australia that sequenced the entire genome of antigenic variant of a coronavirus of chickens. During his 42-year research career as a molecular virologist, immunologist and epidemiologist, he has made critical advancements in understanding the ecology of viral pathogens, led efforts to improve detection and surveillance of viral diseases and developed new and effective vaccines and vaccine strategies to protect commercially reared chickens as well as pathogens, such as avian influenza viruses, which have spilled over into human populations. His research has had a profound impact on practices used today to reduce the incidence and severity of viral diseases of commercially reared poultry as well in human populations.